The world’s largest vaccination drive is currently underway in India.
From March 1, the programme will be extended to the country’s private hospitals for the first time under the next phase of immunisation for senior citizens and persons with comorbidities. For a few months now, the entire vaccination rollout in the country has been reminiscent of the country’s once notorious government-controlled economy, where the government has been undertaking the initiative, keeping the private sector at bay.
That’s also probably why the pace of vaccination has been laggard, forcing clarion calls from India’s top business leaders to allow participation. “If the government was to engage private industry quickly, we can rest assured that we can achieve a coverage of 500 million people within 60 days,” Azim Premji, the chairman of Wipro, told India’s finance minister Nirmala Sitharaman in a post budget interaction. “That"s a practicality. It is important that the government consider this as a major supplementation to the effort.”
This week, the government finally provided some reprieve and permitted private hospitals in the country to start vaccinating large swathes of the population. Ever since the vaccination began on January 16, it has only been the government that has purchased the vaccines and even administered them to close to 3 crore health care and frontline workers.
![vaccine and private sector-1 vaccine and private sector-1]()
In early January, India had given emergency use authorisation to two Covid-19 vaccines, Covishield, manufactured by Pune-based Serum Institute of India, and Covaxin, manufactured by Hyderabad-based Bharat Biotech International Ltd. The government had purchased Covishield at Rs 200 per dose while Covaxin was being purchased at Rs 206. On January 16, the country started the first phase of nationwide vaccination, administering the vaccines to frontline workers and healthcare workers.
“If you think about it in cricket terms, the entire exercise has been similar to allowing only four people in a team to play the opposing team,” Viren Shetty, the chief operating officer of Narayana Health says. “About 70 percent of the health care capacity in India is held by the private sector and they can be instrumental in reducing hesitancy and speed up the process. It would be far more helpful to allow the private sector to procure vaccines and offer options. There are enough manufacturers to procure vaccines from.” Narayana Health is a PMJAY-empanelled hospital.
The government will work out a system that will make vaccine rollouts easy and efficient in the coming days, says Ranjan Pai, chairman, Manipal Education and Medical Group (MEMG). “Because eventually, a Covid-19 shot will be like a normal flu vaccine, to be taken on an annual basis,” he says. “On our end, we have put protocols in place. We have the capacity to administer 25,000 doses every day, which can be ramped up to 50,000 based on demand.”
Under the second phase of vaccination, vaccines would be free of cost at government facilities and for a charge at many private hospitals. “The second phase of the world’s largest vaccination drive will start from Monday in which anybody above 60 years, that may not be less than 10 crore people in the country, and 45 years plus with comorbidities will be given vaccines in 10,000 government medical facilities and also over 20,000 private hospitals,” Prakash Javadekar, India’s minister for Information & Broadcasting said on February 24. “Whoever goes to the government centre will be administered a vaccine free of cost. The Indian government will pay for them. The government will purchase the necessary doses and will send them to all the states.”
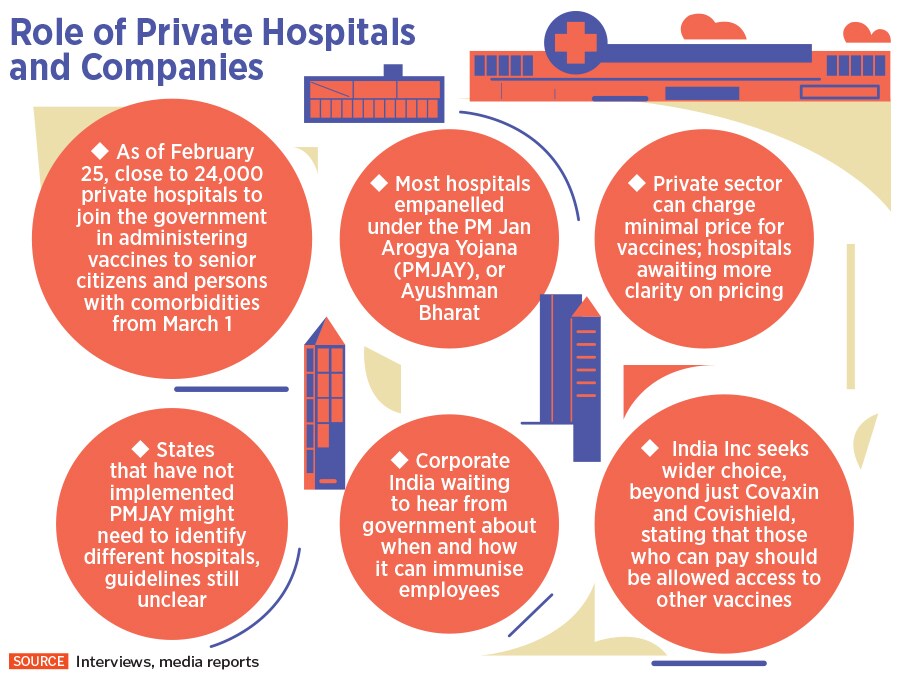
The Centre allocated Rs35,000 crore for Covid-19 vaccines in the Union Budget on February 1. Then, on February 24, the government announced that 24,000 private hospitals, empanelled under the Pradhan Mantri Jan Arogya Yojana (PMJAY), or Ayushman Bharat, will be tasked with administering the Covid-19 vaccine in the upcoming immunisation phase.
The government is currently in talks with manufacturers and hospitals to fix the rates at which it will sell the vaccines. Expectations are that the vaccine will be priced around Rs 400, with Rs 300 going towards vaccine cost and Rs 100 towards administration charges. However, Randeep Guleria, director of the All India Institute of Medical Sciences, has said that the pricing might only be on the overhead expenses borne by the hospital.
"Charges would be to just cover overhead expenses which private sectors would need. Some of which may include cost of syringes and human resources like it was done for testing where charges were fixed to ensure that those aren’t misused and the private sector also doesn’t suffer loss,” Guleria was quoted as saying by news agency ANI.
How the next phase of rollout will work
The next phase of rollout beginning on March 1 will require beneficiaries to register themselves on the government-owned Co-WIN platform. Apart from Co-WIN, the government is also looking at Aarogya Setu, call centres, common service apps and Co-WIN web portals to facilitate registrations.
“There will also be a walk-in provision for the beneficiaries to get themselves registered at a nearby session site to get vaccinated,” R S Sharma, chairman of Empowered Group on Covid-19 Vaccine Administration had told the Press Trust of India.
![vaccine and private sector-2 vaccine and private sector-2]()
To begin with, India will halt vaccinations on February 27 and 28, to upgrade the Co-WIN app, the mainstay of the vaccination programme. The Co-WIN app is a digital platform for real-time monitoring of Covid-19 vaccine delivery and distribution. On this Saturday and Sunday (27th and 28th February), the Co-WIN digital platform will be transitioning from Co-WIN1.0 to Co-WIN 2.0,” India’s health ministry said in a statement. “In view of this, Covid-19 vaccination sessions will not be scheduled during these two days. The states and UTs have been already informed about this transition.”
The new version of the Co-WIN app will have an OTP-based self-registration component that will help the beneficiaries choose the inoculation session site at government or private hospitals.
Family members can also be registered using this account. There is an option for residents of one state to get inoculated in another state, while people aged above 45 years with co-morbidities will have to upload a medical certificate. While the full list of comorbidities is yet to be released, it will include conditions like hypertension, diabetes, kidney and lung diseases, cardiovascular diseases and cancers.
A few appointment slots will also be open for those opting for walk-in registrations. “You can use somebody else’s phone as well, so you need not have a smartphone yourself. On one mobile phone, you can make four appointments,” Sharma told NDTV, adding that while Co-WIN will be integrated to the Aarogya Setu app, people can also access it through an application like the common service app.
The common service centre app was launched for village level tracking of activities by the Common Services Centres (CSC), a multiple-services-single-point model for providing facilities for multiple transactions at a single geographical location, and was launched as part of the Digital India programme in order to help rural or remote areas that did not have access to the internet.
At present, India has close to 2.5 lakh CSCs across 6 lakh villages. Now, under the next phase of the Covid-19 vaccination plan, people from remote rural areas can head to their nearest CSCs for registration. “There will also be the web portal of the Co-WIN app. And there will be IVRs [Interactive Voice Response] and call centres,” Sharma added.
Why India needs the private sector
India is currently the second worst Covid-19 hit country in the world with over 11.1 million cases. In the past few days, cases in the country have been on a rise, particularly in Maharashtra and Kerala.
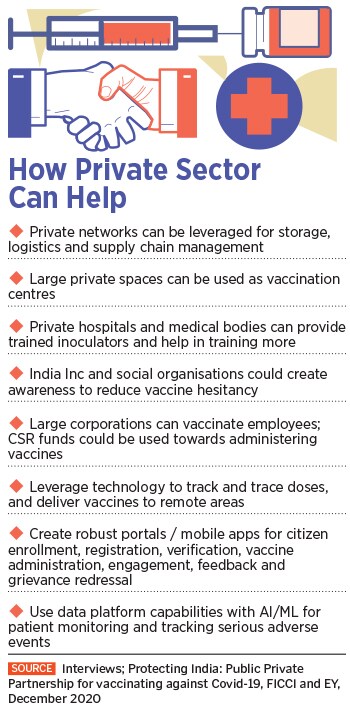
The challenge of administering the vaccine has been formidable for a country like India, given the large population, geographical spread and skewed health infrastructure across urban and rural areas, says Kaivaan Movdawalla, partner-health care, EY India. “In that context, getting into a public-private partnership and leveraging technology becomes very important,” he says.
![vaccine and private sector-3 vaccine and private sector-3]()
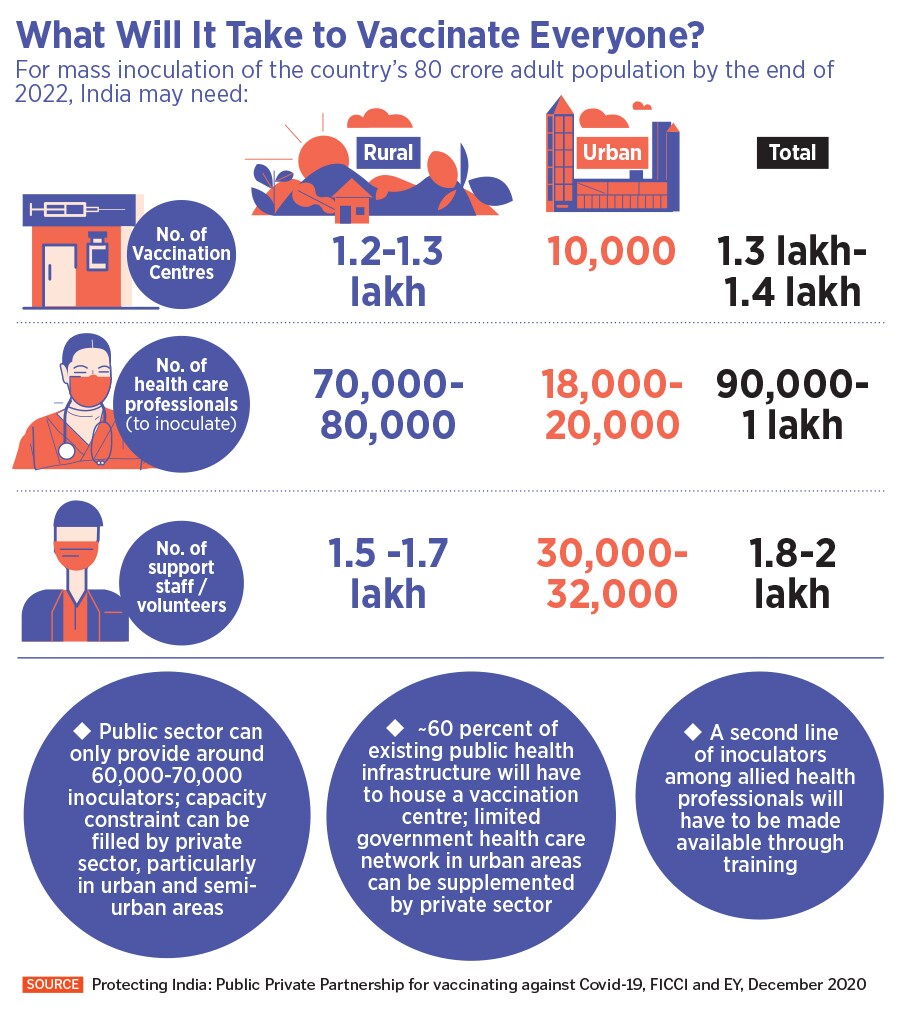
According to a December 2020 strategy paper by FICCI and EY, titled ‘Protecting India: Public Private Partnership for vaccinating against Covid-19’, India needs close to 1 lakh inoculators to administer the vaccine. Out of this, the public sector can only provide close to 60,000-70,000. The capacity constraint, therefore, has to be filled by the private sector, particularly in the urban and semi-urban areas, where there is limited government health care network. “Additionally, a second line of inoculators among allied health professionals will have to be made available through training and credentialing process,” the paper says.
Movdawalla says that participation of the private sector will also be crucial to ensure implementation and monitoring of safety protocols, and keep a check on fraudulent practices. While Artificial Intelligence and Machine Learning can be used to monitor patients for the safety and efficacy of vaccines, blockchain can be deployed to maintain security of personal health and vaccination data.
Yet, vaccine hesitancy and low turnout in recent times have become concerns for the government, something that the private sector can help mend. “The glitches in the process of mandatory registration on the application were among the prominent reasons for the low turnout of health care workers [in Phase 1 and 2],” says Prem Sharma, founder, DayToDay Health, which provides end-to-end patient management solutions.
The startup is among the top four entities shortlisted by the government for the ‘Grand Challenge on Strengthening Co-WIN’ launched in December 2020, which called third-party companies to assist and enable the Co-WIN system. This included innovations and solutions to address infrastructure issues, gaps in cold chain systems and logistics, monitoring and management of vaccinations, and mechanisms to address adverse effects among people who receive the vaccination.
“We would work closely with the government to further strengthen an effective and capable vaccination drive, if selected as the two service providers,” Prem Sharma tells Forbes India. At the time of writing the story, the names of the top two service providers are unclear. According to him, working closely with private, third-party health tech players could help the government prevent glitches that slowed down the vaccination drive for health care and frontline workers.
“Due to technical glitches, beneficiaries did not receive intimations, or correspondence, about the allocated centres and time of vaccination. Another significant downside was the incoming traffic which could not be supported by the application. This resulted in slow loading of data at the vaccination centres, which overhauled the whole process,” he explains.
Prem Sharma adds that verifying credentials on the Co-WIN app and cross-referencing them with Aadhaar also proved challenging to states, while unavailability of on-the-spot registrations caused further delays. “Third-party service providers can not only bring their expertise on board, but can also help in bringing down the turnaround time, as innately their own service mechanisms are robust and easy to scale,” he says.
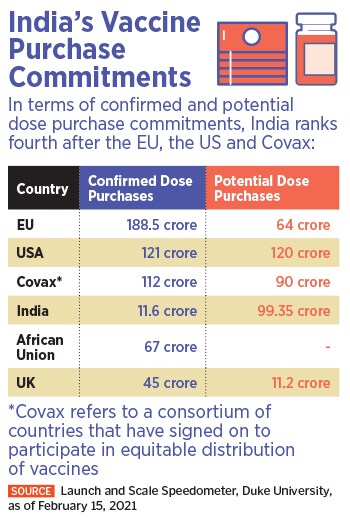
Meanwhile, those being administered the vaccine will not be given a choice between Covaxin and Covishield, a norm that India Inc hopes will change by the time the government tells private corporations how and when they can vaccinate their employees.
![vaccine and private sector-4 vaccine and private sector-4]()
“Let people take responsibility for their own health and be given a choice of which vaccine they want to take, especially if they can pay for it,” says Arvind Mediratta, CEO of Metro Cash & Carry India, which has undertaken to vaccinate all its employees and is in talks with Karnataka state government and central government officials to vaccinate close to 1.2 crore kirana store owners on priority in the upcoming phase of the immunisation programme.
Mediratta, who is also the chairman of the retail and internal trade committee at FICCI, adds that his takeaways from conversations with business representatives of the retail sector indicate that there is hesitancy among many people with respect to the efficacy of the existing vaccine candidates. “We have requested the government that vaccination should not be made mandatory for those who do not want to take it, and those who are ready to pay for vaccination, should be given an option beyond just Covishield and Covaxin.”
Pai of MEMG adds that while having a choice of vaccines would be preferable, his advice would be to “go ahead and get vaccinated with the vaccines the government is making available right now”.

 A frontline health worker gets vaccinated against Covid-19 at sector 30 district hospital, on February 19, 2021 in Noida, India.
A frontline health worker gets vaccinated against Covid-19 at sector 30 district hospital, on February 19, 2021 in Noida, India.