It’s been five months since India rolled out what was touted as the world’s largest vaccination programme. Yet, numerous flip-flops, ranging from policies on procurements to approvals for vaccines, continue to plague the inoculation drive even though the country remains the world"s largest vaccine maker.
India has, so far, fully vaccinated about 4 percent of its population. Of its approximately 94 crore people above the age of 18, only 4 crore, or about 4.25 percent, have been fully vaccinated. As of June 9, a little over 20 percent have received at least one shot.
In contrast, over 42 percent of the US population have been fully vaccinated so far, while at least 63 percent in Israel have received one jab. Across Europe, over 30 percent in various countries have been vaccinated.
Meanwhile, India has now set an ambitious target of vaccinating all of its population above the age of 18 by December. By the looks of it, that’s going to be a Herculean task, especially considering the laggard pace so far.
India has a population of over 134 crore. The country has been vaccinating at an average of 16 lakh doses a day since launching the vaccination drive about 145 days ago. If the government wants to finish vaccinating all the 94 crore adults above the age of 18 by December, that number needs to go up almost five times.
![]()
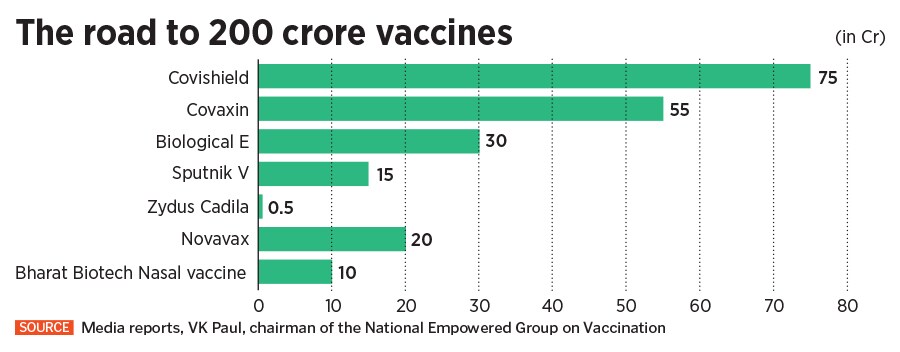
For now, the government has over 53 crore doses of vaccines available with it. If it has to provide over 200 crore doses by the end of this year, in addition to supply from domestic makers, it will also have to bank on supplies from the West, likely to kick in by August. “Vaccine supply will be increasing in the coming days. Seven companies in the country are producing different vaccines, three vaccine trials are at advanced stages," PM Narendra Modi said in a televised address on Monday.
Says KR Antony, a public health consultant, “We need 47 lakh population coverage per day as against coverage of 20 lakh per day because the vaccine production is only that much. There’s a huge deficit, so we have to be pragmatic." According to him, the government’s changing vaccine strategies, including opening up vaccination to all adults when even the priority groups had not received their second dose, and then transferring responsibility to states when there were no vaccines available for purchase was like “declaring a war without armoury".
The government now claims to have secured 74 crore doses for use from August. That includes 25 crore doses of the AstraZeneca vaccine, commonly known as Covishield manufactured by the Pune-based Serum Institute of India, and 19 crore doses of Covaxin, developed and manufactured by Hyderabad-based Bharat Biotech. “All together, 74 crore doses have been secured for use from August onwards," VK Paul, the chairman of the National Empowered Group on Vaccination, said at a press conference on Tuesday. In addition, the government has also secured 30 crore doses from Hyderabad-based Biological E for its vaccine that is currently being developed.
![]()
“It is a difficult task, and a Herculean one," says Nandakumar Jairam, chairman and group medical director at Columbia Asia Hospitals. “But it is possible if we can increase the vaccines and the people who administer them."
The move to procure the vaccines, meanwhile, came after weeks of confusion surrounding the vaccine policy. Modi, in his first televised address on June 7 following the deadly second wave between April and May, reversed an earlier policy announced a month ago. “The Centre is taking back total control of vaccination now, and it will be implemented in the next two weeks. The Centre will give free vaccines to states for all above 18," he said.
“The announcement that, at least in principle, India as a national government takes the responsibility of providing free vaccines to all in a pandemic is a welcome, albeit a small step," says Satyajit Rath, a scientist at the National Institute of Immunology and adjunct professor at the Indian Institute of Science Education and Research. The decision of rolling back the previous policy is partially welcome, although it is a case of ‘better late than never’, according to him. “Sadly, it seems that much of this decision-making is driven by image-related concerns, rather than by a practical focus on driving vaccination forward," he says.
Need to Streamline
The plan to purchase vaccines directly came a month after the government had devolved responsibility to the state governments to procure vaccines. That policy meant half of all vaccines produced in India went to the central government, and the rest to state administrations and private hospitals.
That has now been changed with the central government buying 75 percent of all vaccines, and the state governments receiving their doses for free instead of negotiating directly with manufacturers. “The policy change could have definitely come a little earlier and could have been proactive, nevertheless it is the right way to go," adds Jairam.
The move follows several other flip-flops in the vaccine policy since the government began the programme on January 16 with Covishield and Covaxin. The country had initially set a target to vaccinate 30 crore people, including health care and frontline workers, senior citizens, and persons with comorbidities by July, before vaccinating everyone else.
About 45 days later, the government on March 1, opened up vaccinations to anyone above the age of 60, or above 45 years and with existing comorbidities, to receive vaccines at government as well as private hospitals. That decision marked a significant shift, with the rollout for the general public being moved up, and a long-pending demand to allow the private sector to participate in the programme. At that time, the government didn’t have adequate stock to meet the growing demand, and the manufacturers too hadn’t ramped up capacity.
Under the second phase, vaccines would be free at government facilities and for a charge at many private hospitals. Then, on April 18, the Centre departed from its original plan and put the states and the private sector in charge. Since then, numerous states such as Rajasthan, Madhya Pradesh, Uttarakhand, Tamil Nadu, Maharashtra, Karnataka, Andhra Pradesh, Telangana, Haryana, and Delhi decided to float tenders, inviting global participation in procuring vaccines.
This decision also came in the wake of the the Drugs Controller General of India (DCGI) approving a third vaccine, Russia’s Sputnik V, for emergency use in India. The first batch arrived in India on May 1 and a regulatory clearance was given by the Central Drugs Laboratory in Kasauli on May 13. Hyderabad-based Dr Reddy’s, which has a distribution agreement with the Russian Direct Investment Fund (RDIF)—the sovereign wealth fund of the Russian government responsible for selling the Sputnik V vaccine—did a soft launch on May 14.
The RDIF has tie-ups with five pharma companies in India, which takes the tally of Sputnik V vaccines manufactured in the country to over 85 crore doses. This makes India the biggest global producer of the vaccine, which is developed with two human adenoviral vectors and has an efficacy of 91.6 percent. Dr Reddy’s has a separate deal with Raichur-based Shilpa Medicare to manufacture 5 crore doses of Sputnik V, taking the total production to over 90 crore doses in India.
On May 1, when India began vaccinating its entire adult population, which is close to 70 percent of 136 crore people, under a “liberalised" vaccine strategy that placed greater responsibility on the states, Covid-19 cases had begun to peak, and states were desperate to procure vaccines. “Indian states left to compete/fight with each other in the international market…" Delhi’s Chief Minister Arvind Kejriwal had said about the plan.
This move caused confusion and perhaps affected the efficiency of the inoculation process, says Anant Bhan, a global health, bioethics and health policy researcher. “The impact of the decision on overall vaccination pace would be a question mark, because there are other limiting factors such as supply issues, and other uncertainties like difficulty in delivering vaccines, difficulty in finding slots etc. Sometimes, even if you got slots, you reached the vaccination site only to find out there are none available," he says. “All this could have been avoided if we had a more efficient system where we knew we were working with limited supply and figured out the best way to deliver it, while expanding our supply capabilities. Hopefully, now, we can avoid this going forward."
Under the new vaccine policy, the Centre has also said 25 percent of vaccines will continue to be procured by private hospitals, which are free to charge for the vaccines. As of now, the the per-dose prices at private centres have been fixed at Rs 780 for Covisheld, Rs 1,410 for Covaxin and Rs 1,145 for Sputnik V. The government has said it will monitor prices and strict action will be taken against any private vaccination centre or hospital charging more.
Will These Help?
“All of these [policies] are reactive in nature, as far as I can see," says Rath. “I do not think the original decision of extending vaccination to everyone was well supported by the supply situation. To cap that with what amounted to a responsibility-abrogating decision to make state governments as well as the private market buy vaccines was compounding the error."
Bhan says the new policy is obviously not going to be the only answer considering crucial challenges like inequity in access to vaccines, supply constraints etc. “But the policy might bring more efficiency and clarity in negotiations with manufacturers, because procurement will be from the central government and states won’t have to compete with each other some of the smaller states were struggling because of finance and other constraints under the previous policy," he says.
Rath agrees. According to him, while the new policy will smoothen out purchase negotiations and somewhat improve supply to states, “the competing private procurement, so long as the current situation of vaccine shortages continues, is likely to continue to be a small but significant drag on public vaccination campaigns and to add to vaccine inequities," he says. “Until the supply situation begins to improve, which it might in another month or so, realities on the ground are unlikely to change immediately."
The Centre needs to be honest and transparent about vaccine availability at every stage and the time it will actually take to inoculate everybody, particularly because the country has been lagging behind in its inoculation targets, says Dr Antony, pointing out that less than Rs 5,000 crore out of the Rs 35,000 crore budgetary allocation towards vaccination has been spent so far.
He further suggests that while Bharat Biotech is ramping up its own production capacity, one way to expand production quickly will be to use the 11 public sector units for production of the indigenous vaccine. “These units can be equipped with basic technology and infrastructure, and if Bharat Biotech transfers the technology, these PSUs can turn into production centres that can make enough Covaxin in the country."
Bhan believes the ideal public health response, in view of looming inequities in vaccine access, is to make the vaccines free. “And only if you had enough vaccines, you could divert it to the private sector for those who can pay. But in the absence of adequate supply, where various health systems are competing with each other for [a piece of] a limited pie, it is not the most efficient way," he says.
According to him, since people with financial resources and technological access will have the option of both corporate hospitals and primary health care centres depending on slot availability on the CoWin app, the policy, as it stands, will lead to them cornering slots or procuring doses faster those bereft of the privilege. “Why create this inequity in the first place is the question mark. Because you could use the private sector as delivery points, but it would still be key that you do not charge the beneficiary. That’s not the way we’ve gone about it."

 A healthcare worker injects a shepherd with Covishield vaccine during a vaccination drive at a forest area in south Kashmir"s Pulwama district, June 7, 2021 Image: Danish Ismail / Reuters[br]
A healthcare worker injects a shepherd with Covishield vaccine during a vaccination drive at a forest area in south Kashmir"s Pulwama district, June 7, 2021 Image: Danish Ismail / Reuters[br]